CQV-Commissioning Qualification & Validation
GAMP Group offers Complete Food Plant Commissioning, Qualification & Validation includes Temperature Distribution, Heat Distribution and Heat Penetration Studies.
CQV (Commissioning, Qualification, and Validation) is a very detail-oriented process that requires the right mix of knowledge, experience, and diligence to correctly place equipment/systems into use.
Additionally, with global food authorities’ regulations and requirements continually changing, it is crucial to understand the CQV lifecycle to remain compliant.
Our dedicated CQV engineers bring wide-and-deep knowledge of the entire validation lifecycle to support all major sectors within the Food, Medical Devices, Pharmaceutical and Life Sciences industry. We guide you in the selection of the right validation strategy and fully support all your tactical, hands-on deliverables, from protocol preparation, through “floor executions” and data analysis.
GAMP Group’s CQV services includes:
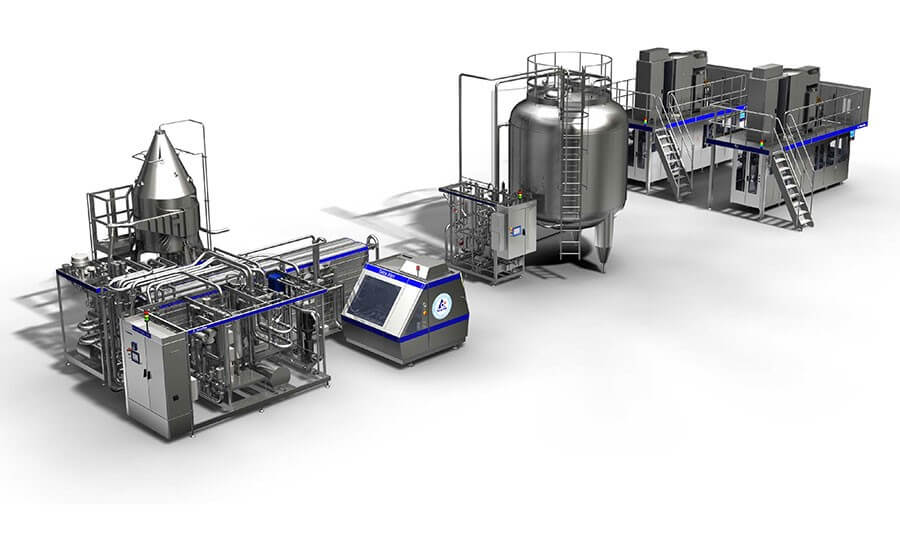
1. Commissioning of facilities, utilities and equipment like
- Retort
- Lyophilizer
- Aseptic filling lines
- Packing lines
- HVAC & Water Utilities
2. Qualification and Validation (Q&V) of facilities, utilities, equipment and computerized systems;
3. Support to Process Validation activities;
4. Support to Analytical Methods Validation activities;
5. Support to Cleaning Validation activities;


FDA/Regulatory Requirements for Aseptic Processing and Packaging
The U.S. Food and Drug Administration (FDA) defines aseptic processing and packaging as: "The filling of a commercially sterilized cooled product into pre-sterilized containers, followed by aseptic hermetical sealing, with a pre-sterilized closure, in an atmosphere free of microorganisms." 1
Current Good Manufacturing Practices (cGMPs): Aseptic processing facilities must adhere to cGMP guidelines outlined by FDA. This involves maintaining hygienic conditions, proper equipment maintenance, employee training, stringent cleaning, sanitation, and quality control measures. However, aseptic processing and packaging goes beyond regular cGMPs, and a specific HACCP-based program must be implemented. Aseptic processing is very complex, and all equipment, packaging, and products must reach a state called "commercial sterility" in which no microorganisms can grow under the planned storage conditions.
Cleaning and Sanitation: Before starting aseptic processing and packaging lines, it is imperative that they are free of any residues, microbes, and contaminants, thus ensuring a sterile environment. Clean-in-place (CIP) and sterilization-in-place (SIP) processes are imperative prior to starting production to achieve and uphold commercial sterility, safeguard product integrity, and meet stringent regulatory and industry standards. These processes must be well validated and carefully monitored.
Qualification ,Validation and Documentation: Manufacturers must thoroughly validate every step of their aseptic processing and packaging control and documentation systems. Validation involves demonstrating that the system consistently achieves the desired level of sterility, even under adverse circumstances. Companies must routinely maintain detailed documentation of processes, packaging, equipment, sanitation, and maintenance procedures and records during production.
Sterilization Parameters: FDA requires that all equipment, packaging, and products be "commercially sterile," which means free of any microorganism that can spoil the product or make people sick. As such, a thermal process authority must be responsible for the safety of the product and specify precise sterilization parameters, including temperatures and times, to ensure the elimination of harmful microorganisms while preserving the quality of the product.
Packaging Integrity: Aseptic packaging is generally flexible, and strict requirements exist to ensure the integrity of packaging materials and their ability to maintain sterility throughout the product's shelf life.
Monitoring Deviations: Continuous monitoring of the aseptic processing and packaging system is essential to promptly identify and address any deviations from established parameters. This includes monitoring critical control points (CCPs) such as sterilization temperatures, filling rates, and packaging integrity. Any deviations from the specified parameters can indicate potential risks to product safety and quality, requiring immediate corrective action to prevent contamination and ensure compliance with regulatory standards.
Scheduled Process: A process is selected by the processor as adequate under the conditions of manufacture for a given product to achieve commercial sterility. This process may be in excess of that necessary to ensure destruction of microorganisms of public health significance and shall be at least equivalent to the process established by a competent processing authority to achieve commercial sterility. Manufacturers must follow a scheduled process prepared by a competent thermal process authority, which includes specific heat treatments and control measures to maintain commercial sterility to ensure the safety of products.
Process Filing with FDA and Compliance: A detailed process filing must be submitted to FDA, outlining the aseptic processing methods, equipment used, sterilization parameters, and validation data. Compliance involves strict adherence to the approved process. Each product must be filed with FDA. The filing documents must contain the following components:
- The thermal process
- Equipment sterilization and maintenance of sterility
- Filling and packaging machine validation
- The final product, which has been validated using a combination of microbiological and physicochemical tests.
This follows a comprehensive food safety plan, which includes thorough recordkeeping of critical factors. Data from all CCPs must be monitored and recorded.
Recordkeeping and Monitoring: Due to the complexity of aseptic processing and packaging, recordkeeping and monitoring of several CCPs during each step of production, cleaning, and sanitation are essential for ensuring compliance and demonstrating the safety of products. Validated electronic data recorders are essential to ensure continuous monitoring of each control point, as well as management of deviations and alarms.
Validation of Aseptic Processing and Packaging System
Validation plays a pivotal role in the aseptic process, and aseptic systems must operate under an always validated state. Validation is a continuous process that involves a series of tests and procedures to ensure that the processing and packaging systems consistently achieve the desired level of sterilization. This includes meticulous monitoring of CCPs, equipment calibration, maintenance records, and thorough documentation to verify that the system retains the effectiveness and reliability of the entire process achieved at the validated state.
Achieving Commercial Sterility
Commercial sterility of equipment and containers used for aseptic processing and packaging of food is defined by FDA as "the condition achieved by application of heat, chemical sterilant(s), or other appropriate treatment that renders the equipment and containers free of viable microorganisms having public health significance, as well as microorganisms of non-health significance, capable of reproducing in the food under normal non-refrigerated conditions of storage and distribution."1 A hermetically sealed container is defined as a "container that is designed and intended to be secure against the entry of microorganisms and thereby maintain the commercial sterility of its contents after processing." 1
The goal of aseptic processing is to achieve commercial sterility, which means that the product and packaging are free of any microorganism that can grow under the standard storage conditions. This ensures that the products remain free from harmful and spoilage microorganisms throughout their shelf life. This is achieved through a precise combination of time, temperature, and proper packaging, which maintains the integrity of the products without compromising their safety.
Quality of Ingredients, Raw Materials, and Packaging Materials
The quality of ingredients, raw materials, and packaging materials is integral to the success of aseptic processing. Any deviation from quality standards at any stage of production can compromise the entire process. Rigorous quality control measures must be in place to ensure that only the finest materials are used, minimizing the risk of contamination and preserving the quality of the final product.
Microbiological Quality and Food Safety
Microbiological quality and food safety are non-negotiable aspects of aseptic processing. The scheduled process is prepared to ensure that commercial sterility is achieved. Stringent testing and monitoring are conducted throughout the process to detect and eliminate any potential sources of contamination. This ensures that the final product meets the highest safety standards and poses no risk to consumers.
It is normal practice to test a few samples for positive release; typically, a few samples are incubated for 7–14 days to ensure there are no off-odors or observable package bloating. Even though the aseptic processes are validated, it is a good idea to have the in-house microbiology lab perform aerobic plate count (APC) and yeast/mold tests to rapidly detect defects in post-processing and package closures. If the product is low-acid, then the quality assurance tests should include mesophilic and thermophilic anaerobic spores, which are the hardest to eliminate and which have the potential to produce Clostridium botulinum. 2
Rapid Microbiological Testing
In recent years, the dairy and plant-based beverage industry has witnessed a significant shift toward the use of rapid microbiological testing methods, such as ATP bioluminescence technology, flow cytometry-based technology, and classical media microbiology. These innovative approaches have emerged as reliable alternatives to traditional plate microbiological testing, particularly for evaluating aseptic and extended shelf life (ESL) products.
ATP bioluminescence technology has quickly gained traction and is now considered the industry standard for the rapid microbial screening of ultra-high temperature (UHT) aseptic and ESL dairy and plant-based beverage products. Its widespread adoption is attributed to its efficiency, accuracy, and ability to provide quick results, enabling manufacturers to streamline their quality control processes.
One of the key advantages of ATP bioluminescence technology is its ability to significantly reduce testing time and product hold times. Traditionally, microbiological testing using plate methods could take anywhere from 7–14 days. In contrast, ATP bioluminescence technology reduces this timeframe to 48 hours or fewer. This accelerated testing process allows for faster release of products into the market, minimizing inventory costs and improving overall operational efficiency.
Nutritional and Organoleptic Quality
Aseptically processed and packaged foods and beverages aim to retain their nutritional value and sensory attributes. Technology preserves the natural flavors, textures, and nutritional content of the products, providing consumers with high-quality options that are both safe and nutritious.
Shelf Life of Aseptically Processed and Packaged Products
One of the significant advantages of aseptic processing is the extension of product shelf life stored and handled at ambient temperature. Properly processed and packaged products can have an extended shelf life without the need for preservatives or refrigeration, ensuring freshness and quality over an extended period of time.
Finished Product Positive Release Criteria
Before aseptically processed food and beverage products are released for distribution and sale, they must meet specific criteria to ensure that they adhere to regulatory requirements and consumer expectations. Positive release criteria typically include adherence to predetermined microbiological standards, confirmation of proper sealing and packaging integrity, and compliance with established quality parameters. Only products that meet these criteria are deemed safe and suitable for consumption, thereby safeguarding consumer health and maintaining the reputation of the manufacturer.
This program also applies to the procedures for releasing quarantined or held product. These procedures might include outlining process measures that demonstrate products are compliant with specified requirements, or that products not meeting the specifications are safely disposed.



 Copyright GAMP Services 2024. All Rights Reserved.
Copyright GAMP Services 2024. All Rights Reserved.